Benefit Checks
View estimated out-of-pocket costs, alternative medications, pharmacy dispensing options, and insurance coverage details
Photon recently added a real-time benefit check feature to our prescriber experience. When writing an Rx for a patient who has benefits on file, we'll run a coverage check as a prescription is added to an order.
The results are based on the patient’s benefit, pharmacy, and treatment. Coverages will come back with one of three statuses:
- Covered - this status will display a co-pay amount
- Covered with Restrictions
- Not Covered
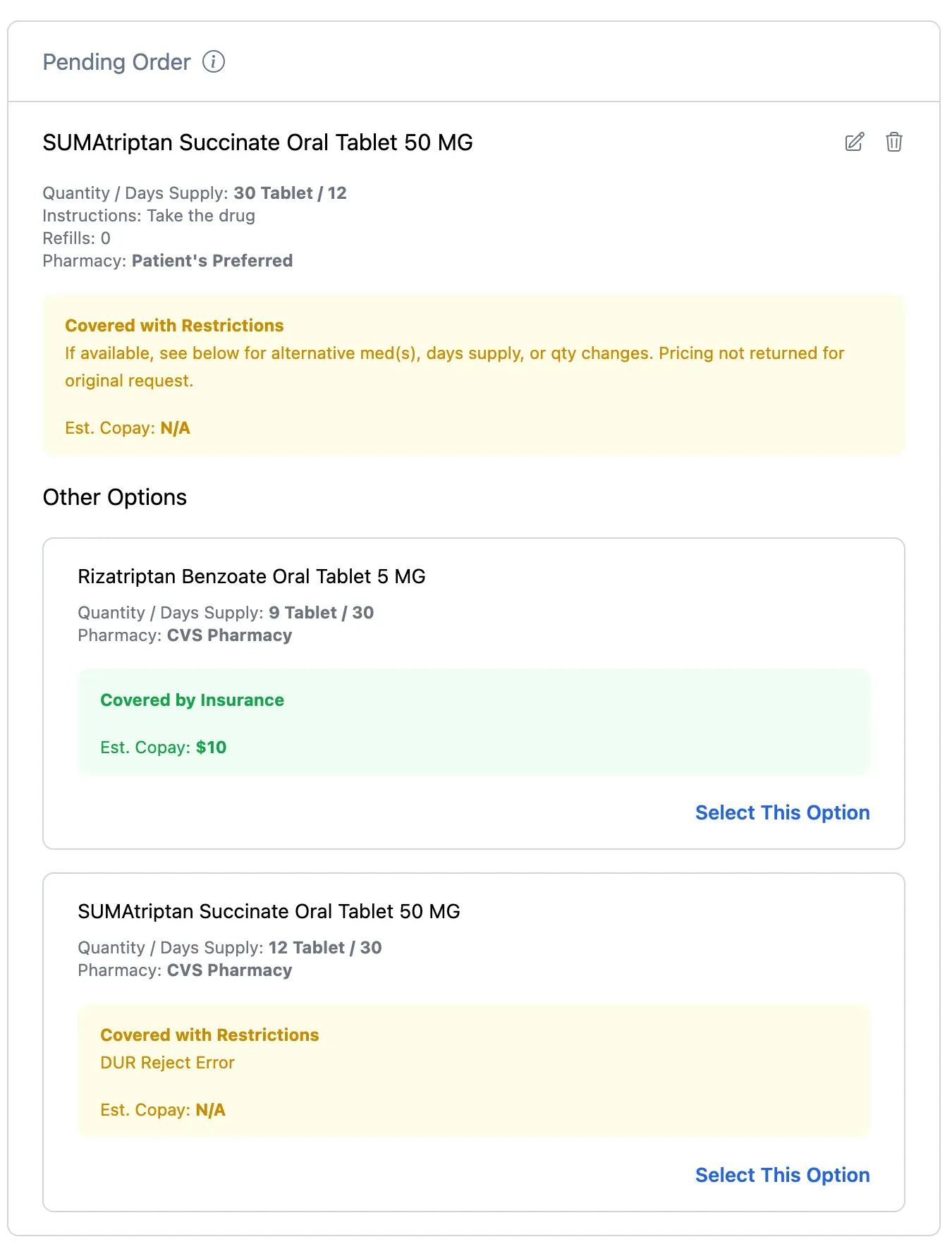
Benefit check example response on a pending order
Often, a coverage check will show “Other Options”. These might be therapeutic alternatives or different pharmacies. By clicking “Select This Option”, the original will be removed, and the form pre-populated with that option’s values. The selected Pharmacy will also be updated, if different for that option.
Creating Patient Benefits
In order to generate a coverage check the patient will need to have a benefit associated with them. You can do this with the Patient Benefits API.
See the Patient Benefits API reference documentation here.
Configuring Photon Elements
In order to display the coverage checks, make sure your version of Elements is v0.16.0 or higher. Enable the feature by setting the enable-coverage-check to true:
<photon-prescribe-workflow
enable-coverage-check="true"
...
></photon-prescribe-workflow>Understanding Coverage Statuses
Covered by insurance
A “covered by insurance” status indicates to the provider the requested medication is on the payer’s formulary, is covered by the patient’s plan, and the patient should expect to pay the amount shown in the estimated copay response. This status will always include a copay. It is important to note the copay amount can vary depending on the plan and any deductible the plan requires.
Covered with restrictions
We’ll show various statuses in a yellow banner that fall under this category if the insurance indicates there is coverage but there are additional restrictions.
- PA required
- The quantity and/or days supply of the medication requires
adjustment to be within plan limits (e.g., Quantity Limit Exceeded) - A refill is too soon or not fillable until a certain date
- A diagnosis code is required with the prescription
- Any other restrictions the plan may have in place (e.g., age
requirements)
These scenarios will include additional messaging that will be displayed to the provider indicating details about the restriction and how it can be resolved. These responses can include a patient pay amount (e.g. if a PA is required).
Not covered by insurance
A not covered response status will appear in a red banner and may indicate the medication is not covered and/or the patient’s preferred pharmacy may be out-of- network. This may include a copay amount. When it includes a copay, this is typically the fee charged to the patient for a non-formulary medication.
This response will generally return a list of alternative medications or pharmacy-(ies) covered by the patient’s plan. A patient pay amount will also show for each alternative.
Coverage Alerts
The following coverage alerts may be returned beneath the coverage status and status message. These are subject to change at the discretion of the PBM with new alerts being added regularly. We’ll show these messages in the alert to the provider.
-
Age Restrictions Limit
-
Exceeds Day Supply Limit
-
Medication Not Covered
-
Excessive Utilization
-
Cost Not Fully Covered
-
Gender Restrictions Apply
-
Generic Medication Required
-
Not On-Formulary
-
Out-of-Network Pharmacy
-
Plan Limitations Apply
-
Dispense Quantity Restrictions Apply
-
Exceeds Dispense Quantity Limit
-
Invalid Dispense Quantity
-
Step Therapy Requirements Apply
-
Coverage Message from Payer
Updated 3 months ago
